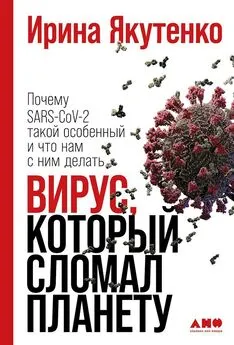
Ирина Якутенко - Вирус, который сломал планету. Почему SARS-CoV-2 такой особенный и что нам с ним делать
- Название:Вирус, который сломал планету. Почему SARS-CoV-2 такой особенный и что нам с ним делать
- Автор:
- Жанр:
- Издательство:Альпина нон-фикшн
- Год:2021
- Город:Москва
- ISBN:978-5-0013-9400-6
- Рейтинг:
- Избранное:Добавить в избранное
-
Отзывы:
-
Ваша оценка:
Ирина Якутенко - Вирус, который сломал планету. Почему SARS-CoV-2 такой особенный и что нам с ним делать краткое содержание
Что мы знаем о SARS-CoV-2, почему он убивает одних и бессимптомно проходит у других, безопасна ли вакцина и когда будет найдено лекарство, как мы лечим COVID-19 без него, можно ли бороться с патогеном, не закрывая планету, — книга отвечает на эти и многие другие вопросы. Хотя пандемия еще не закончилась, и мы все время получаем новые данные о вирусе, изложенные в тексте фундаментальные основы уже не поменяются: они служат каркасом, на который читатель сможет нанизывать новые знания.
Вирус, который сломал планету. Почему SARS-CoV-2 такой особенный и что нам с ним делать - читать онлайн бесплатно ознакомительный отрывок
Интервал:
Закладка:
169
R. A. Watson et al. , «Reduction of total lung capacity in obese men: comparison of total intrathoracic and gas volumes», J. Appl. Physiol. , vol. 108, no. 6, pp. 1605–1612, Jun. 2010.
170
A. E. Dixon and U. Peters, «The effect of obesity on lung function», Expert Rev. Respir. Med. , vol. 12, no. 9, pp. 755–767, Sep. 2018.
171
X. Zhang et al. , «Systemic inflammation mediates the detrimental effects of obesity on asthma control», Allergy Asthma Proc. , 2017.
172
R. Huttunen and J. Syrjänen, «Obesity and the risk and outcome of infection», Int. J. Obes. , vol. 37, no. 3, pp. 333–340, Mar. 2013.
173
UN Women, «COVID-19: Emerging gender data and why it matters», 2020. [Online]. Available: https://data.unwomen.org/resources/covid-19-emerging-gender-data-and-why-it-matters. [Accessed: 05-Jun-2020].
174
G. H. 50/50, «COVID-19 sex-disaggregated data tracker», 2020. [Online]. Available: https://globalhealth5050.org/covid19/sex-disaggregated-data-tracker/. [Accessed: 18-Aug-2020].
175
C. Karagiannidis et al. , «Case characteristics, resource use, and outcomes of 10 021 patients with COVID-19 admitted to 920 German hospitals: an observational study», Lancet Respir. Med. , Jul. 2020.
176
H. Ueyama et al. , «Gender Difference Is Associated With Severity of Coronavirus Disease 2019 Infection: An Insight From a Meta-Analysis», Crit. Care Explor. , vol. 2, no. 6, p. e0148, Jun. 2020.
177
M. J. Nasiri et al. , «COVID-19 clinical characteristics, and sex-specific risk of mortality: Systematic Review and Meta-analysis», medRxiv , p. 2020.03.24.20042903, Jan. 2020.
178
C. Karagiannidis et al. , «Case characteristics, resource use, and outcomes of 10 021 patients with COVID-19 admitted to 920 German hospitals: an observational study», Lancet Respir. Med. , Jul. 2020.
179
Robert Koch Institute, «Coronavirus Disease 2019(COVID-19)Daily Situation Report of the Robert Koch Institute. 01/06/2020 — UPDATED STATUS FOR GERMANY», 2020.
180
G. H. 50/50, «COVID-19 sex-disaggregated data tracker», 2020. [Online]. Available: https://globalhealth5050.org/covid19/sex-disaggregated-data-tracker/. [Accessed: 18-Aug-2020].
181
C. Vlassoff, «Gender differences in determinants and consequences of health and illness»., J. Health. Popul. Nutr. , vol. 25, no. 1, pp. 47–61, Mar. 2007.
182
A. E. Thompson, Y. Anisimowicz, B. Miedema, W. Hogg, W. P. Wodchis, and K. Aubrey-Bassler, «The influence of gender and other patient characteristics on health care-seeking behaviour: a QUALICOPC study», BMC Fam. Pract. , vol. 17, no. 1, p. 38, Dec. 2016.
183
S. L. Klein and K. L. Flanagan, «Sex differences in immune responses», Nat. Rev. Immunol. , vol. 16, no. 10, pp. 626–638, Oct. 2016.
184
J. E. Fa, J. R. Stewart, L. Lloveras, and J. M. Vargas, «Rabbits and hominin survival in Iberia», J. Hum. Evol. , vol. 64, no. 4, pp. 233–241, Apr. 2013.
185
K. S. Singh, «Gender Roles in History: Women as Hunters», Gend. Technol. Dev. , vol. 5, no. 1, pp. 113–124, Mar. 2001.
186
M. T. Dorak and E. Karpuzoglu, «Gender Differences in Cancer Susceptibility: An Inadequately Addressed Issue», Front. Genet. , vol. 3, 2012.
187
M. McCarthy, «The ‘gender gap’ in autoimmune disease», Lancet , vol. 356, no. 9235, p. 1088, Sep. 2000.
188
L. Yan et al. , «An interpretable mortality prediction model for COVID-19 patients», Nat. Mach. Intell. , vol. 2, no. 5, pp. 283–288, May 2020.
189
D. M. Del Valle et al. , «An inflammatory cytokine signature predicts COVID-19 severity and survival», Nat. Med. , Aug. 2020.
190
X. Xu et al. , «Effective treatment of severe COVID-19 patients with tocilizumab», Proc. Natl. Acad. Sci. , vol. 117, no. 20, pp. 10970–10975, May 2020.
191
G. Gritti et al. , «IL-6 signalling pathway inactivation with siltuximab in patients with COVID-19 respiratory failure: an observational cohort study», medRxiv , p. 2020.04.01.20048561, Jan. 2020.
192
W. Gou et al. , «Gut microbiota may underlie the predisposition of healthy individuals to COVID-19», medRxiv , p. 2020.04.22.20076091, Jan. 2020.
193
J. Zhao et al. , «Relationship between the ABO Blood Group and the COVID-19 Susceptibility», medRxiv , p. 2020.03.11.20031096, Jan. 2020.
194
M. Zietz and N. P. Tatonetti, «Testing the association between blood type and COVID-19 infection, intubation, and death», medRxiv , p. 2020.04.08.20058073, Jan. 2020.
195
D. Ellinghaus et al. , «The ABO blood group locus and a chromosome 3 gene cluster associate with SARS-CoV-2 respiratory failure in an Italian-Spanish genome-wide association analysis», medRxiv , p. 2020.05.31.20114991, Jan. 2020.
196
Z. Wang et al. , «Influences of ABO blood group, age and gender on plasma coagulation factor VIII, fibrinogen, von Willebrand factor and ADAMTS13 levels in a Chinese population», PeerJ , vol. 5, p. e3156, Mar. 2017.
197
L. Gallinaro et al. , «A shorter von Willebrand factor survival in O blood group subjects explains how ABO determinants influence plasma von Willebrand factor», Blood , vol. 111, no. 7, pp. 3540–3545, Apr. 2008.
198
C. A. Latz et al. , «Blood type and outcomes in patients with COVID-19», Ann. Hematol. , vol. 99, no. 9, pp. 2113–2118, Sep. 2020.
199
K. Hennig, «(21) Coronavirus-Update: Antikörpertests kommen bald», NDR Info — Das Coronavirus-Update mit Christian Drosten , 2020.
200
C. Menni et al. , «Real-time tracking of self-reported symptoms to predict potential COVID-19», Nat. Med. , May 2020.
201
UK Department of Health and Social Care, «Statement from the UK Chief Medical Officers on an update to coronavirus symptoms: 18 May 2020», 2020.
202
L. Mao et al. , «Neurological Manifestations of Hospitalized Patients with COVID-19 in Wuhan, China: a retrospective case series study», medRxiv , p. 2020.02.22.20026500, Jan. 2020.
203
J. Y. Tong, A. Wong, D. Zhu, J. H. Fastenberg, and T. Tham, «The Prevalence of Olfactory and Gustatory Dysfunction in COVID-19 Patients: A Systematic Review and Meta-analysis», Otolaryngol. Neck Surg. , p. 019459982092647, May 2020.
204
D. Pierron et al., «Smell and taste changes are early indicators of the COVID-19 pandemic and political decision effectiveness», Nat. Commun. , vol. 11, no. 1, p. 5152, Dec. 2020.
205
«Рост за неделю — больше 40 процентов». О чем говорит динамика ковидных поисковых запросов, Фонтанка. Ру , 12-Oct-2020.
206
A. S. Bhattacharjee, S. V. Joshi, S. Naik, S. Sangle, and N. M. Abraham, «Quantitative assessment of olfactory dysfunction accurately detects asymptomatic COVID-19 carriers», EClinicalMedicine , p. 100575, Oct. 2020.
207
D. H. Brann et al. , «Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia», Sci. Adv. , vol. 6, no. 31, p. eabc5801, Jul. 2020.
208
Y. Lee, P. Min, S. Lee, and S.-W. Kim, «Prevalence and Duration of Acute Loss of Smell or Taste in COVID-19 Patients», J. Korean Med. Sci. , vol. 35, no. 18, 2020.
209
E. N. Antonova, C. E. Rycroft, C. S. Ambrose, T. Heikkinen, and N. Principi, «Burden of paediatric influenza in Western Europe: a systematic review», BMC Public Health , vol. 12, no. 1, p. 968, Dec. 2012.
210
V. Usonis et al. , «Central European Vaccination Advisory Group (CEVAG) guidance statement on recommendations for influenza vaccination in children», BMC Infect. Dis. , vol. 10, no. 1, p. 168, Dec. 2010.
211
WHO, «Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19)», 28-Feb-2020.
212
J. S. Brownstein, K. P. Kleinman, and K. D. Mandl, «Identifying Pediatric Age Groups for Influenza Vaccination Using a Real-Time Regional Surveillance System», Am. J. Epidemiol. , vol. 162, no. 7, pp. 686–693, Oct. 2005.
213
E. Miller, K. Hoschler, P. Hardelid, E. Stanford, N. Andrews, and M. Zambon, «Incidence of 2009 pandemic influenza A H1N1 infection in England: a cross-sectional serological study», Lancet , vol. 375, no. 9720, pp. 1100–1108, Mar. 2010.
214
D. F. Gudbjartsson et al. , «Spread of SARS-CoV-2 in the Icelandic Population», N. Engl. J. Med. , vol. 382, no. 24, pp. 2302–2315, Jun. 2020.
215
F.-C. Zhu et al. , «Safety, tolerability, and immunogenicity of a recombinant adenovirus type-5 vectored COVID-19 vaccine: a dose-escalation, open-label, non-randomised, first-in-human trial», Lancet , vol. 395, no. 10240, pp. 1845–1854, Jun. 2020.
216
R. M. Viner et al., «Susceptibility to SARS-CoV-2 Infection Among Children and Adolescents Compared With Adults: A Systematic Review and Meta-analysis.,» JAMA Pediatr., Sep. 2020.
217
I. Dattner et al. , «The role of children in the spread of COVID-19: Using household data from Bnei Brak, Israel, to estimate the relative susceptibility and infectivity of children», medRxiv , p. 2020.06.03.20121145, Jan. 2020.
218
F.-C. Zhu et al. , «Safety, tolerability, and immunogenicity of a recombinant adenovirus type-5 vectored COVID-19 vaccine: a dose-escalation, open-label, non-randomised, first-in-human trial», Lancet , vol. 395, no. 10240, pp. 1845–1854, Jun. 2020.
219
C. M. Szablewski et al. , «SARS-CoV-2 Transmission and Infection Among Attendees of an Overnight Camp — Georgia, June 2020», MMWR. Morb. Mortal. Wkly. Rep. , vol. 69, no. 31, pp. 1023–1025, Aug. 2020.
220
«Första resultaten om antikroppar efter genomgången covid-19 hos blodgivare», Folkh ä lsomyndighetens , 16-Jun-2020.
Читать дальшеИнтервал:
Закладка:
![Арсений Сухоницкий - Эмгед Гард / Мне достался божий сценарий и я не знаю, что с ним делать. Том 2 [СИ]](/books/1060982/arsenij-suhonickij-emged-gard-mne-dostalsya-bozhij.webp)
![Арсений Сухоницкий - Эмгед Гард / Мне достался божий сценарий и я не знаю, что с ним делать [СИ]](/books/1060984/arsenij-suhonickij-emged-gard-mne-dostalsya-bozhij.webp)
![Илья Мартынов - Мозг. Как он устроен и что с ним делать [litres]](/books/1074310/ilya-martynov-mozg-kak-on-ustroen-i-chto-s-nim-del.webp)